Are you ready to take charge of your health?I help women achieve vibrant health through all phases of life with a personalized, holistic approach.
Sign up for my newsletter and get your Free Gift:
A Smart Woman's Guide to Hormone Balance
Sign up for my newsletter and get your Free Gift:
A Smart Woman's Guide to Hormone Balance

Struggling with constipation can feel frustrating, especially when your daily bowel movements aren’t satisfying. Healthy stools are crucial, yet often overlooked. In my practice, I frequently discuss stool patterns with clients, covering everything from frequency to shape, color, and consistency. After all, we’re all aware when something feels “off.”
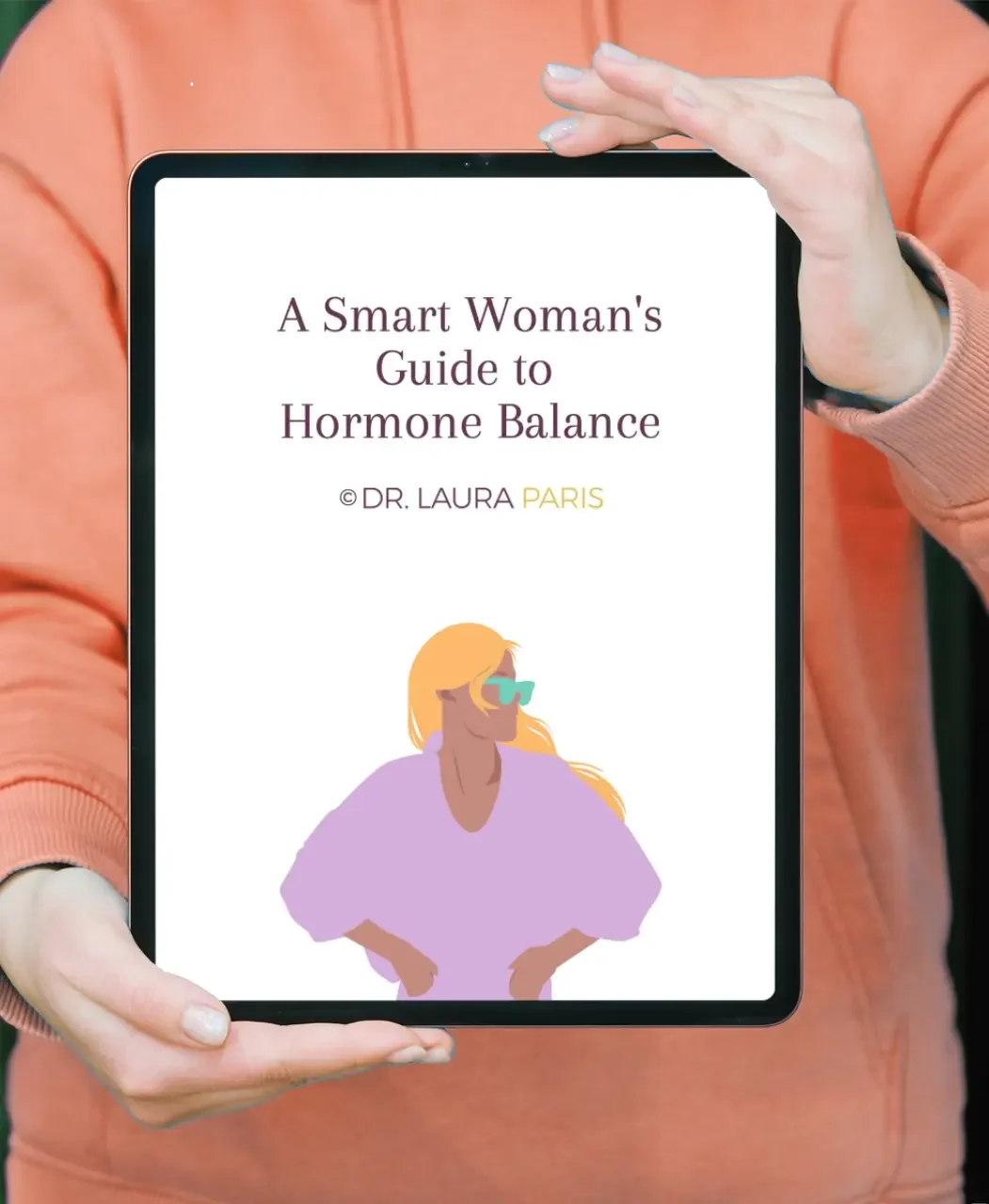
A helpful tool we use is the Bristol Stool Chart, a clinical resource for identifying stool types. Types 1 and 2 indicate constipation, types 3, 4, and 5 are healthy (with 4 being optimal), and types 6 and 7 indicate diarrhea. Let’s focus on the constipated types and explore root-cause solutions.
The traditional medical definition of constipation is:
“Constipation is generally described as having fewer than three bowel movements a week.”
But who feels good only going three times a week? From a functional medicine perspective, constipation refers to incomplete or infrequent bowel movements on a daily basis. You’re functionally constipated if you:
Ideally, a bowel movement should be like any healthy animal: sit, relax, gently push, and you’re done in under five minutes. If this doesn’t sound like you, you may be functionally constipated.
Constipation can impact your health by allowing waste products to sit too long in your colon, which may lead to toxin reabsorption, gut bacteria imbalances (dysbiosis), altered pH levels, and even colon cancer.
Start by consulting a doctor to rule out any physical colon or rectal issues. Next, check your hormone levels, as imbalances—especially low thyroid—can contribute to constipation. Pregnancy and certain medications can also cause constipation.
You can test your transit time—the time it takes for food to move through your system. Ideal transit time is 12-24 hours; more than 24 hours is slow, and over 48 hours means waste is sitting in the colon for too long. To test, consume ½ to 1 cup of red beets or take four charcoal tablets. Red stools mean the beets have passed, and black stools indicate the charcoal. This will show how long your food takes to move through.
If you have slow transit time and experience significant abdominal bloating, you may have small intestine bacterial overgrowth (SIBO). This occurs when bacteria grow in the wrong part of your gut. Constipation can be both a cause and an effect of SIBO, and this condition typically leads to bloating that worsens throughout the day.
To test for SIBO, try following a low-FODMAP diet. If your symptoms improve, SIBO may be the issue. Consult a gastroenterologist or functional medicine practitioner for a breath test to confirm.
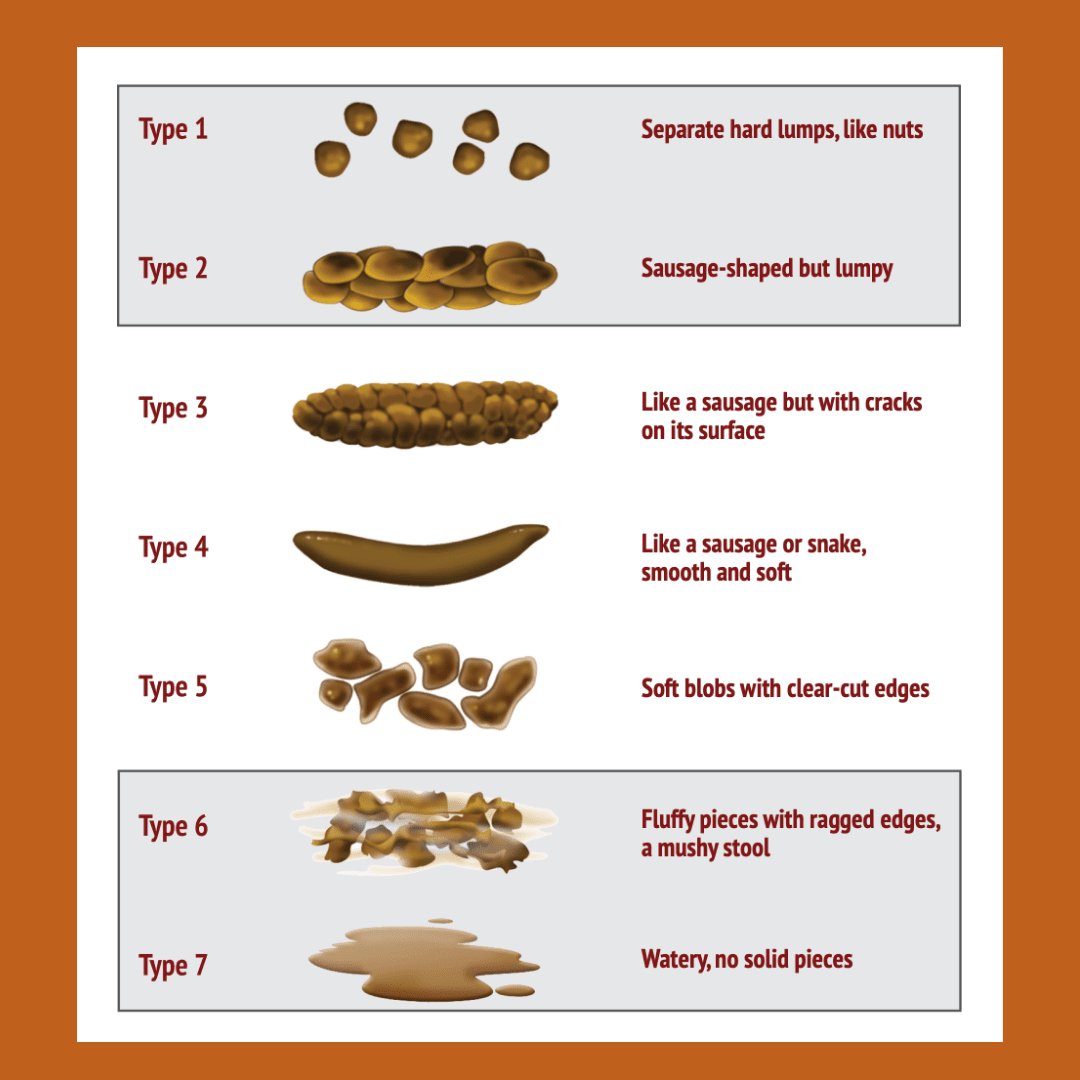
Dysbiosis, on the other hand, refers to an imbalance in your gut bacteria, which can include yeast, viruses, and parasites. A GI-MAP functional stool test can help identify which microbes are out of balance, so you can address the problem accurately.
Constipation can also result from deficiencies. You might lack movement, fluids, fiber, stomach acid, digestive enzymes, beneficial gut bacteria, or magnesium. These factors are key to achieving a healthy stool score of type 4. Here’s how to identify and address possible deficiencies:
Constipation often stems from a combination of root causes. It’s best to implement these changes one at a time and observe how your body responds. For more complex cases, ordering a GI-MAP stool test can help uncover deeper imbalances in your gut. Once your test results are available, we can work together in a new patient consultation to interpret them and create a personalized treatment plan to resolve your constipation for good.
Comments about this topic? Please share in the comments below,

Dr. Laura Paris is a women’s health specialist who provides Acupuncture and Functional Medicine care at her two clinics in Capitola and Monterey, California. She also works with women remotely in the United States through telehealth appointments. Learn more about Laura here, and message her directly here.
Click the button to talk to Dr Laura on a 20-minute discovery phone call ($67)